A Doctor Describes the Sanctity of Life In the Sunset Years
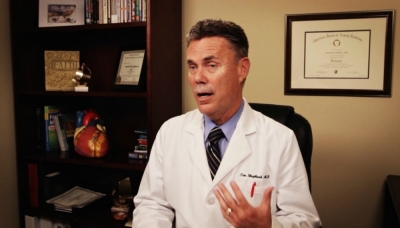
As a physician, my calling is to promote life. I have pledged to uphold the sanctity and dignity of human life as part of the Hippocratic Oath.
It is unethical to have quickening death as an option. Yet this year alone, half of our nation's state legislatures have proposed legalizing the practice of a person taking deadly drugs to end their life prematurely. A new Gallup poll shows that 56 percent of Americans now find euthanasia "morally acceptable."
These trends concern me. In taking a life, you are grasping the keys out of God's hands. That is not my place as a doctor, one who has given my life to help heal people.
Life is very precious, and every day is a gift. I have a patient in a nursing home whom I have been seeing for 20 years, who has severe multiple sclerosis. He is quadriplegic, completely paralyzed from the neck down, though he can interact with others – including his seven daughters, who visit him ever so often.
This man is the happiest person you will ever meet. Every time I go into his room, he has a smile on his face. The nursing home staff love bringing him to the lobby, where he encourages and cheers on other patients. He speaks to every person who comes by.
My staff and I follow the medical principles of acute care in treating this patient: every number outside the norms of health, we need to deal with. We make a problem list, and we try to solve each issue with a treatment plan.
In 30 years of practicing medicine, I have also walked alongside many families who face a different situation later in life. Consider a man who comes to the point when he is 86 years old, on multiple medications, suffering from congestive heart failure, in and out of the hospital multiple times over the past month – that man is miserable. He can barely walk from his bed to the bathroom.
Whatever time he has left, our desire as loved ones is to honor him and cherish every moment. "Wisdom is found with the elderly, and understanding comes with long life," says Job 12:12.
There is such power in listening – to their stories, yes, and also to their needs. What most seniors want in these situations is to stay in their own place, rather than moving to a facility. It's called aging in place.
At first aging in place may simply be living an active lifestyle, hopefully with children or grandchildren nearby who are checking in and enjoying life with grandpa. Then at some point the senior may transition to needing hospice care, which essentially provides medical care in the home.
I have had patients who did not want to consider hospice because they thought I was talking about physician-assisted suicide. I tell them frankly: "I don't kill anybody; that is never the goal of medical care. You've worked hard your whole life, you've paid taxes – I want you to get the services you paid for. Hospice is a help to you and it's 100 percent paid. This is going to make your life a lot simpler."
Two of my elderly patients live nearby on a little ranch. He is an old Texas boy; he and his wife have cows and live the ranch lifestyle. Yet now they are not safe to drive themselves anywhere.
They could sell their ranch and move into a nice assisted living home. But they want to stay on their little ranch and tend to their cows – it is their life, they have the freedom to live it fully.
By choosing to go on hospice, now we have people who keep an eye on them. Nurses and aides go out to see them and fill in around the edges so they can continue to live well as long as possible. The patient is happy, and the family is happy.
Statistically, people who go on hospice live longer than people who choose not to go on hospice. Nurses and aides take care of those little problems. If an elderly person catches a cold that turns into pneumonia, he may not get out of his bed – there have been situations where, tragically, a person was found deceased days later.
When a nurse is watching for these issues, she will take action: "You are sick, let's speak to the doctor about getting an antibiotic." He gets better, does not contract pneumonia, and lives much longer. People love this option.
A fully competent senior should be able to address end-of-life issues with her family doctor. This discussion certainly requires bonds of trust between those involved: I am present as her doctor (to promote her longevity and wellness), then the spouse, and at some point children may be involved or whomever the senior designates.
Ultimately this will come around to big questions such as, What is it you want to have done for you, and not to have done? It is a difficult conversation; we navigate it only by keeping the value of life at the forefront.
If a cancer patient says, "I don't want to do chemotherapy or surgery," we recognize they have the right to make that choice. They have the right to refuse care. In those sunset years, our cherished grandparents face a similar set of choices.
People can say, "This is the way I want to be treated. These are the things I want to have done: I do (or do not) want to have a ventilator, or to be shocked, or to have a feeding tube." A competent person can request not to have certain things done to them – medical staff will follow the directives a senior has made, as well as what is ethical in the situation.
I have had people in a feeding-tube situation, where a treatment plan is proceeding well; one would certainly not pull the tube out and end someone's life, as occurred with Terri Schiavo in Florida. It was a very unusual case, especially considering she was only 41 years old and maintaining vital functions on her own.
As a physician, I am committed to saving my patient's life; I have no right to take her life.
In the final stage of life, the principles of palliative care provide us a path – instead of treating every single problem, our goal is to treat problems to keep the patient comfortable.
There is a sacredness to dying. It is a privilege to take care of people during that time. Think about it from a Christian standpoint: this person is about to be right before Jesus, sitting in the throne room within a few minutes.
A family can have that assurance. Often it is harder for the family to let them go than it is for the person. There are many goodbyes to say. Why make it any more horrific for the family than you have to? Making a unilateral decision about when you die hurts them.
Doctors and nurses help keep people comfortable at the very end, we don't want them to be in pain – those are steps to honor a person and treat them with dignity.
Life is a gift from God: He gives it, and He takes it away.
Reprinted with permission from Bound4LIFE.