Making end-of-life decisions: The problems with advance directives

We’re all going to die one day. Are you prepared? Yes, for heaven, but also, have you made decisions about how to handle your medical care?
So what did your family discuss this past Christmas Eve? The beautiful lights? Maybe some childhood holiday memories? Hopefully, the immeasurable gift of the Incarnation and the love of God?
Well, according to the online medical journal STAT, you should have talked about the importance of advance medical directives. As Dave Barry likes to say, I’m not making this up.
In an article published on, of all days, Christmas Eve, STAT told readers that advance directives are a “perfect holiday conversation.” Yep, break out the eggnog…
If you’re unfamiliar with the term, an “advance directive” is “a legal document in which a person specifies what actions should be taken for their health if they are no longer able to make decisions for themselves because of illness or incapacity.” The most basic example of an advance directive is a “do not resuscitate” order. There are also more complex ones, like “living wills,” that specify what kind of treatment the person will or will not receive.
While I disagree that Christmas is the best moment for this discussion, STAT is absolutely right to say that people should be thinking about their medical care and should be discussing it with their loved ones. As bioethicist Wesley J. Smith notes, preparing an advance directive is “an important task given the evolving economics of medicine.”
But as Smith and others have pointed out, there are far more than merely economic considerations to be discussed. Our plans for the end of our lives ought to carefully reflect our deepest convictions about the sanctity of human life from conception to natural death.
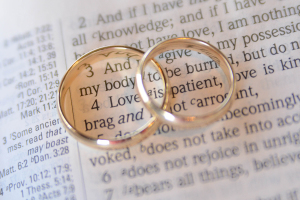
Done badly, an advance directive can be like a prenuptial agreement. Just as a “prenup” assumes the impermanence of marriage, many advance directives create a presumption in favor of death and efficiency (and an all-out avoidance of suffering) over the sanctity of human life.
Watch the language, and beware whenever the term “quality of life” as defined by medical professionals is elevated over the “sanctity of life” inherent to all image bearers. And especially look out for economic undertones in advance directives. Economically-driven decisions about the end of life will only reflect and advance the culture of death. This is especially true when directives use broad and imprecise language, which many do—language that opens the door to a purely utilitarian approach to end-of-life care.
And here’s another problem: Many advance directives operate as if our lives belong only to ourselves, as if all that matters is what we want when it comes to pain, suffering, or treatment. This ignores what they think. And by “they,” I mean the husbands who belong to their wives, and vice-versa, the parents who belong to their kids and vice-versa, and all of us who belong to extended families, communities, and churches.
Then there’s this: Years can pass between the writing of an advance directive and death. So you might be subjecting your loved ones to a decision you made long ago, when they have more information about the options than you ever knew about. Just as a life lived in pure autonomy never ends well, neither does a death.
Fortunately, there are alternatives to advance directives and living wills. One of these is what’s called a “durable power of attorney,” which designates a trusted person—a friend or a family member—to handle your affairs if you become mentally or physically incapacitated. The key word here is “trusted,” someone with whom you share convictions about the sanctity of human life and who is prepared to act on them even in the face of pressure.
This keeps decisions about care out of the sole hands of hospitals or doctors who might embrace an agenda or belief system diametrically opposed to yours.
I understand … this isn’t the most pleasant of subjects. But “it is appointed to men to die once and after that comes judgment.” This knowledge should prompt us to want to not only live, but to die as well as we can, bearing witness to our convictions about Whose we are and Whom we serve.
And be sure to check out today’s BreakPoint podcast. Warren Cole Smith speaks with Ben Mitchell about end-of-life decisions, advance directives, and the growing threat (and popularity) of doctor-assisted suicide.
Tune in at BreakPoint.org or wherever you listen to podcasts.
Resources
We’re making it too hard to have a ‘good’ death, Joshua A. Rolnick, David A. Asch, and Scott D. Halpern | STATnews.com | July 5, 2017
The End-of-Life Bureaucracy, Wesley J. Smith | The Weekly Standard | December 7, 2015
Patients Rights Council website
Talking about advance directives is a perfect holiday conversation, Kenneth R. White | STATnews.com | December 24, 2018
Originally posted at Breakpoint.