Justice for Our Forgotten Neighbors
Global poverty, sex trafficking, slavery, unfair wages, child labor, environmental exploitation. I'm proud to see and support Christians confronting these and other injustices, as an expression of our faith and calling. I'd also love for more Christians to be aware of a need close to home, affecting many of our own friends and neighbors. In our efforts to meet the needs of people in well-publicized peril, most of us are not hearing a cry for justice within our own mental-health system.
Did you know that people living in poverty are at greater risk for mental illness, and vice versa? "It's a vicious circle where both poverty seems linked to greater rates of mental illness, and in some cases, certain kinds of mental illness seem linked to a greater likelihood of living in poverty," says John M. Grohol, PsyD.
That's not all.
Among people with mental illness, 60 to 80 percent are unemployed. For people living with the most severe mental illnesses, unemployment can be as high as 90 percent.
About 40 percent of homeless people have some kind of mental health problem, and 20 to 25 percent of homeless people have serious mental illness.
Nationwide, more than half of people incarcerated in local, state, and federal correctional facilities have symptoms of serious mental illness. According to the United States Department of Justice, percentages range from 45 percent of federal prisoners to 56 percent of state prisoners and 64 percent of inmates in local jails. More people with mental illness are housed in Chicago's Cook County Jail than in any psychiatric hospital in this country.
My mother, who has schizophrenia, is part of this statistic. She is not a violent or habitual criminal, but she has spent time in both local jail and federal prison. Many others, like her, are not a threat to society when healthy; they simply failed to receive appropriate mental-health intervention before committing crimes. Sadly, for many going to jail is the only way to finally get the care they need, but they never should have ended up there.
How We Got Here
From the 1950s through the 1970s, the mental-health care system underwent a massive deinstitutionalization, a well-intentioned plan designed to move people out of hospitals and into local communities. In theory, community-based services would replace the large state-run institutions and provide more flexibility, a more personal touch, and the freedom to engage in society. Unfortunately, local communities largely failed to provide the necessary services for all the people sent their way. They also failed to address the stigma and prejudice regularly aimed at those affected by mental illness.
In more recent decades, families have found themselves stymied by strict privacy laws, legal hurdles to committing a loved one to care, and insurance limitations. Unless someone presents a clear and immediate danger to self or others, no one can compel another person to receive mental-health treatment. So when they see a problem approaching, family members are often powerless to intervene. They're often left out of the circle of care as well. Under current laws, family members--even spouses and parents of adult children--cannot gain access to medical information without the written consent of the person under treatment. In some states, parents must obtain written consent from children starting at age 12. Anyone who has tried to care for a loved one in a mental-health crisis knows how hard it can be to obtain this written consent.
The mental-health care system is difficult to navigate and expensive to access. Insurance companies are reluctant to pay for adequate care. Many psychiatric medications are terribly expensive. And our society perpetuates a stigma attached to mental illness, which keeps people from acknowledging mental-health problems. Because of these and other reasons, experts estimate that around 50 percent of people with serious mental illness do not receive treatment. According to the National Alliance on Mental Illness (NAMI), "Without treatment the consequences of mental illness for the individual and society are staggering: unnecessary disability, unemployment, substance abuse, homelessness, inappropriate incarceration, suicide and wasted lives; The economic cost of untreated mental illness is more than 100 billion dollars each year in the United States." We all pay the price for our neglect.
A Call to the Church
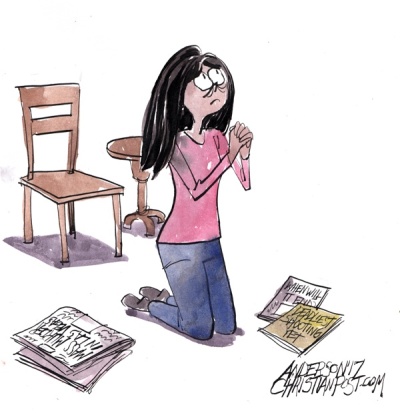
The church is well-positioned to offer both hope and help. We can advocate for better mental-health services. We can support legislation for better funding and insurance coverage. We can get educated and address our own fears and questions so we can reach out to others rather than pretend we don't see them. We can support people affected by mental illness in the same practical ways we support other people with health problems. We can extend our hands in friendship and address the spiritual questions mental illness raises. We can acknowledge Mental Health Awareness Month every May by simply talking about this topic we haven't historically discussed. We can research the gaps in our local communities and make plans to fill those gaps in ways we're qualified to do so.
We have neglected this ministry for too long. This kind of work for justice is much less glamorous than those that involve international travel. It may be less rewarding than the ones where you always see tangible results. It may be less enjoyable than helping people who always say thank you. But it is no less important. And it is something every single one of us is called to do. It's called loving your neighbor.
Amy Simpson is a life & leadership coach, speaker, and author of Blessed Are the Unsatisfied: Finding Spiritual Freedom in an Imperfect World, Anxious: Choosing Faith in a World of Worry, and Troubled Minds: Mental Illness and the Church's Mission (all InterVarsity Press). You can find her at AmySimpson.com and on Twitter @aresimpson.
Originally posted at Amy Simpson.com.